Radicular Pain: What a Spine Doctor Assesses Differently
Key Takeaways
- Radicular pain is assessed by where symptoms travel, not where they are felt most strongly, because direction reveals nerve involvement more reliably than location.
- Consistency and repetition matter more than severity, as mild but predictable pain can signal ongoing nerve compression.
- Movement-triggered symptoms provide clearer diagnostic clues than pain at rest, since nerve-related pain responds predictably to position and activity.
- Sensory changes such as numbness or tingling add critical context, often remaining more stable than pain intensity and helping pinpoint nerve pathways.
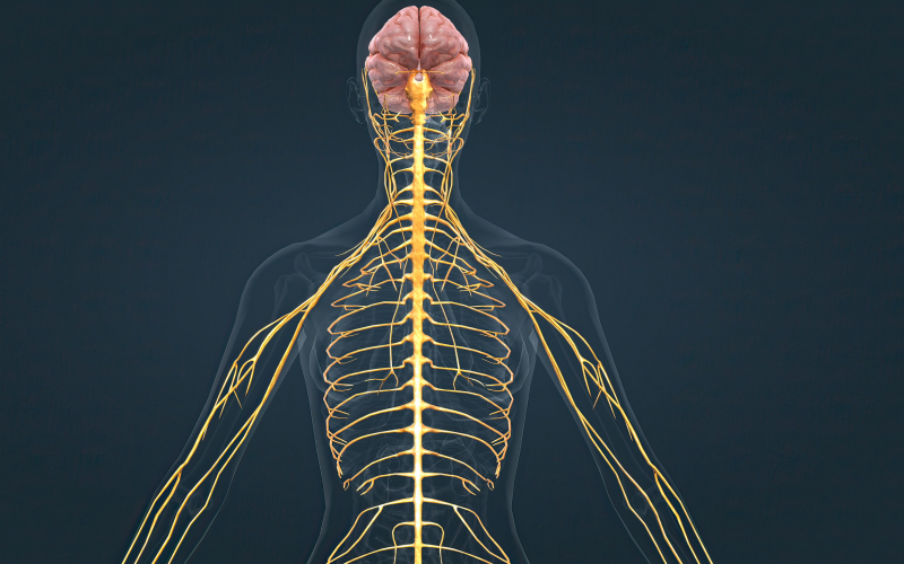
Radicular pain changes how a spine doctor in Singapore approaches assessment because the source no longer corresponds to the spot that hurts, forcing attention away from local strain and toward nerve pathways instead. When discomfort travels into the arm or leg, its direction becomes more informative than its intensity, as repeated radiation often points to compression along a specific nerve rather than isolated tissue irritation. The consistency of the pain’s appearance and location is more important than its intensity on any given day. Rather than the intensity of the pain, radicular pain is determined by how frequently it manifests with specific movements, positions, and daily activities.
1. Pain Location Becomes Less Reliable Than Pain Path
Assumptions about muscular strain or joint irritation that typically remain local are challenged by the fact that radicular pain rarely starts in the area that hurts the most. Instead of focusing on the point of discomfort, a spine doctor follows the direction the pain travels, because patterns that move from the neck into the arm or from the lower back into the leg often trace specific nerve pathways. These travelling patterns carry more diagnostic meaning than isolated tenderness at a single spot, especially when they repeat with movements or positions. Assessment, therefore, shifts away from surface structures and toward how nerve involvement shapes pain behaviour across the limb rather than where it is felt at any one moment.
2. Consistency Matters More Than Intensity
Because mild discomfort might indicate persistent nerve irritation when it follows the same pathway over days and activities, radicular pain does not necessarily need to be severe to merit care. What draws a spine doctor’s focus is not the peak intensity of pain, but its reliability, especially when specific movements, postures, or routines reproduce the same travelling sensation. This repetition separates muscular discomfort, which frequently fluctuates without a regular path or reason, from nerve-related patterns. Consistent discomfort that is nonetheless bearable indicates structural involvement that should be investigated further rather than dismissed.
3. Movement Triggers Carry Diagnostic Weight
Certain movements, such as turning the neck, lifting the arm, or remaining seated for long periods, tend to reproduce radicular pain in consistent ways, which provides information that static symptoms cannot reveal on their own. Because these actions place load or tension along specific nerve pathways, a spine doctor observes how pain responds during movement rather than only at rest. This contrast matters, as radicular pain usually reacts predictably to position changes while local muscular discomfort often eases with warmth, rest, or massage. Tracking these movement-based responses helps narrow the likely source of nerve compression without relying solely on imaging findings.
4. Sensory Changes Add Context Beyond Pain
Radicular pain frequently appears alongside numbness, tingling, or altered sensation, even when discomfort itself feels manageable, which is why these sensory changes carry diagnostic weight beyond pain alone. Rather than signalling simple irritation, shifts in sensation suggest disruption along specific nerve pathways that influence how signals travel through the limb. A spine doctor pays close attention to where sensation changes appear and how they spread, because these patterns often align with particular nerve roots more reliably than pain intensity does. While pain may fluctuate day to day, altered sensation tends to remain consistent, offering a steadier reference point for understanding nerve involvement.
Conclusion
Radicular pain shifts assessment away from where discomfort is felt and toward how it behaves across movement, posture, and time, because travelling symptoms reveal patterns that localised pain cannot explain on its own. Even if pain is still tolerable, discomfort starts to distinguish between nerve involvement and surface strain when it frequently travels the same route into an arm or leg, responds to particular movements, and manifests alongside sensory alterations. The difficulty lies in recognising that consistency carries more meaning than severity, as persistent behaviour can signal compression long before pain becomes disruptive. In this way, radicular pain is understood through repetition and direction, where the body’s responses over time reveal what intensity alone cannot clarify.
Contact Achieve Spine And Orthopaedic Centre to discuss radicular pain when travelling, as symptoms suggest nerve involvement rather than local strain.