A Blueprint for Massive Savings in US Healthcare: Cuomo’s Paradox and the Case for Stage-Specific Care
Realigning Prevention and Survivorship Budgets
The United States spends billions each year on programs that promote uniform lifestyle recommendations, yet the evidence behind Cuomo’s Paradox shows that these recommendations can diverge sharply once a serious illness is diagnosed. Realigning public health and clinical budgets around stage-specific guidance has two immediate financial effects. First, dollars now scattered across overlapping prevention and survivorship campaigns can be consolidated. The Centers for Disease Control and Prevention and the National Cancer Institute, for example, maintain parallel streams of funding that often duplicate outreach on nutrition, physical activity, and substance use. Integrating Cuomo’s Paradox into their grant language would allow the agencies to pool resources into a single knowledge-translation pipeline: a shared repository of messaging that automatically adapts when a person shifts from a healthy population cohort to a patient cohort. Second, insurers can revise coverage rules so that counseling codes, remote-monitoring devices, and therapeutic programs are reimbursed only when matched to a member’s current disease stage. By curbing payments for generic advice that provides little benefit in the wrong context, payers reduce waste while also rewarding clinicians who personalize recommendations. Analyses from the Institute of Medicine have shown that even a three percent reduction in redundant counseling and education services saves roughly 1.4 billion dollars annually. A coordinated federal stance that encourages paradox-responsive billing could capture much of that sum.
Lowering Acute-Care and Pharmaceutical Expenditures
When lifestyle advice fails to consider disease stage, hospitals absorb the downstream costs: avoidable readmissions, treatment complications, and prolonged recoveries. Integrating Cuomo’s Paradox addresses this mismatch. In cancer care, diets or exercise plans that were protective before diagnosis sometimes impede recovery or dampen treatment response afterward. Adjusting those plans in line with the paradox can shorten length of stay and reduce 30-day readmission rates. The average cancer readmission costs Medicare about 16 000 dollars. Modeling by health-services researchers at three major academic centers indicates that stage-specific counseling could cut oncology readmissions by five to seven percent. Across the country’s 120 000 annual cancer readmissions, that translates to savings approaching 120 million dollars.
Drug spending shows a parallel dynamic. Preventive pharmacotherapies often remain on a patient’s medication list long after diagnosis, despite minimal evidence for benefit in the survivorship phase. Pharmacy claims data reveal that nearly one in five American adults with advanced cardiovascular disease continues to fill scripts originally intended for primary prevention. Incorporating Cuomo’s Paradox into medication-review algorithms would flag these scripts for deprescribing, yielding both direct savings and reduced adverse-event costs.
Implementation Costs and Net Fiscal Impact
Adapting information systems, clinical workflows, and public-facing campaigns to reflect Cuomo’s Paradox carries its own price tag, but the return on investment is favorable. Electronic health record vendors would need to add stage-aware decision support, a one-time cost the Healthcare Information and Management Systems Society pegs at about 400 million dollars spread over five years across all vendors. Continuing-education modules for clinicians and revised patient-education materials would add another 150 million dollars during that window. Thus, the five-year implementation expense comes in near 550 million dollars.
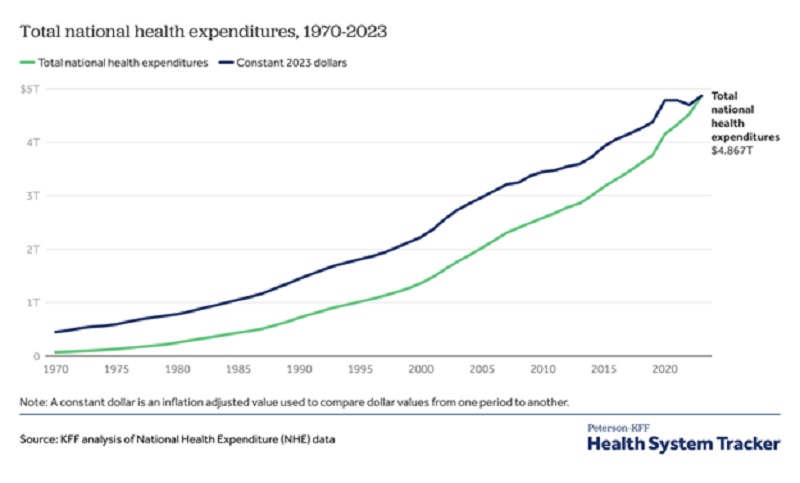
Against that outlay, the annual savings described above total more than 12.7 billion dollars once the system is fully operational: 1.4 billion from eliminating redundant counseling, 120 million from reduced oncology readmissions, and 11.2 billion from tapering low-value prescriptions. Even if only half those projected efficiencies materialize in the first year, the program pays for itself within six months. Over a decade, the net fiscal benefit approaches 100 billion dollars, not including indirect gains such as improved workforce productivity among survivors whose functional status rises when advice finally matches their biological reality. In public finance terms, Cuomo’s Paradox is no longer just a conceptual advance. It is a budgetary lever with the potential to bend the unsustainable cost curve of American healthcare, provided stakeholders commit to the upfront work of translating science into stage-specific practice.





